Latest 2021 data reveals IBS symptoms and diagnosis is much more common during and post Covid-19 lockdown , mainly due to stress. What is IBS and why does latest data reveal such rise? In this short digestible post, you will understand:
Contents
What is IBS?

Irritable Bowel Syndrome is a complication that gives a lot of discomfort to a patient’s abdomen. Ergo, it is defined as a common disorder characterised by chronic abdominal pain specifically associated with a change in frequency or form of bowel habit [2].

Fig.1: Microscopic anatomy of large intestine as histological structure. Many crypts are seen to elongate and extend deeply onto lumenal flat surface, mucosa and muscularis.
A healthy, thus normal body’s waste components after digestion (mouth to small intestine) are deposited as stool in the large intestine region.
However, the stools in the large intestine of IBS patients’ cause pain, discomfort and irritation of the surrounding large intestinal tissues (mucosa, submucosa, musular layer, serosa), refer to Fig.1. This can cause a repeating cycle of diarrhea (severe IBSD), constipation (severe IBSC), both (IBSCD/ IBSMixed/IBSUnclassified) over a time period.
Thus, the Rome criteria divides IBS into these 4 subtypes in terms of the patient’s most prominent bowel habit.

In clinical practice, IBS is one of the most common functional gastrointestinal disorders (FGIDs) [1]. Although IBS in general is more common among women, IBS-D is more common among men [2]. This counts to ~40% of all IBS patients [2].
What causes IBS?
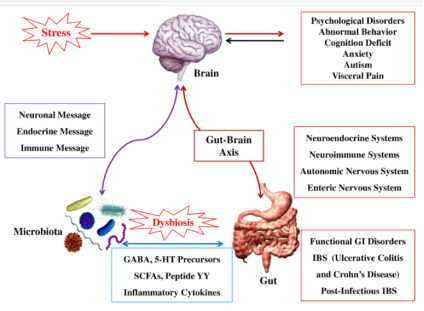
Fig. 2: indicating brain-gut axis interaction; Microbial-host metabolism and the effect on behavioral function of brain. Stress, brain related disorders are the major culprits, with current research, [ Thakur AK, Shakya A, Husain GM, Emerald M, Kumar V (2014) Gut-Microbiota and Mental Health: Current and Future Perspectives. J Pharmacol Clin Toxicol 2(1):1016.]
Though there is no answer yet to why this chronic discomfort occurs, but what is known is this:
There is a communication error between the brain and large Intestine via nerve signals that allow for the regulation of peristalsis. IBS patients have a defect in signalling from the brain to the large intestine (brain-gut axis [2]), resulting in abnormal peristalsis.
Peristalsis: movement of muscle contraction that is always present from the stomach to the large intestine, to regulate digestion.
If there is a slow communication to the large intestine via delayed brain nerves signals: constipation as peristalsis is halted.
If there is a hyperactive communication to the large intestine via hyperactive brain nerves signals: diarrhea as peristalsis has increased much more than required.
Other Factors That Lead To IBS?
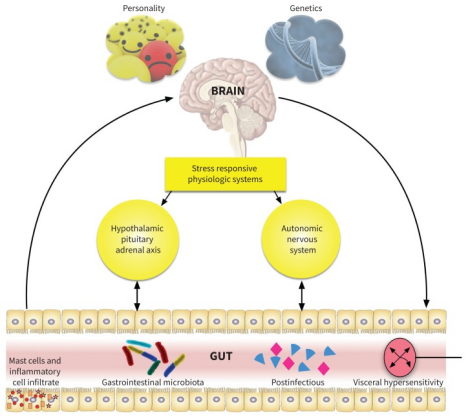
Figure 3: schematic summary of the pathophysiological factors that lead to IBS. Personality (eg. Anxiety,stressful etc.), genetics (ancestrial, inherited traits).
One’s personality– stress is a prominent trait that is associated in terms of the disrupted brain-gut axis communiciation.
Genetic traits– family history of colorectal carcinoma [2]
Dehydration and lack of fibre rich, gut pleasing foods in your diet: Simply drinking more water than usual and consumption of high fibre is required for gut pain relief.
Symptoms?

Irritation: The stools causing irritation in the large intestine commonly cause discomfort, abdomen pain, cramps.
Diarrhea and constipation: Patients describe pain and discomfort either due to diarrhea, constipation or both. Additionally, patients are more likely to experience a cycle of diarrhea and constipation. This occurs over a period of time, usually 6 days.
IBS is a syndrome that prioritises symptomology based on diagnosis using the Rome criteria [1]. This is mainly to biomarker absence. Ergo, this heterogeneity is much more complicated to treat.
Diagnosis:

Controlled Tests are normal yet the patient is experiencig symptoms of IBS:
A patient is classed as IBS if all other contolled tests via The Exclusion Principle are conducted and conclude as normal, yet still experience discomfort and irritation. This is done to exclude any other possible underlying issues relating to the colon and gastrial intestine.
Tests that show normal healthy results in IBS and normal patients:
USG profile, normal stool profile, normal colonoscopy, normal blood tests.#
What to know: IBS differential diagnosis is not specific. Other medical conditions such as inflammatory bowel disease (IBD), bile acid diarrhea, celiac disease and lactose intolerance are interlinked.

No blood is seen in the stool samples:
If there is blood, then IBD (structurally defective small intestine , gastrintestinal tract) may be the diagnosis. For those patients; ferritin, total blood count, vitamin B testing, C-reactive protein inflammatory marker testing is taken into account to confidently distinguish between IBD and iron deficiency anaemia [2].
To Summarise: So, if tests done are normal and the patient consumes a lot of water and has tried taking foods that are great for digestion and constipation (senna and fibre rich foods): IBS classified.
Medical Caution:
The information provided within this post is accurate with credible and reputable sources. However, if the signs of IBS are highly severe, then take further expert advice from your local hospital, GP. Make sure to take all tests mentioned above. Stay Safe!
Treatment

Currently, there is no cure. Treatments are only to manage the irritation. However, first in-line treatment [1] is to adapt a lifestyle change and to tweak your diet:

£6.27 The Clever Guts Diet by Dr Michael Mosley. Clever guts indeed!
Changing your lifestyle and consuming the special natural foods that boost your immune system and gut microbiome (click here to know what Dr Michael Mosley recommends) can reset your gut health , leaving you feeling relieved and less stressed.
You will be surprised by how many patients diagnosed with many medical complications have reduced their symptoms and their effects. How? By resetting their natural microflora.

£11.60 Yakult 15 x 65ml
Consuming probiotics (yakult) and resetting your gut microbiome should treat bowel irritation and pain in the gut. Thus, relieving refractory IBS symptoms.
Alternative treatments:
Hypnotherapy, psychotherapy, phytomedicines and acupuncture are also alternative treatments. However, not enough tests and biomedical research are carried out to determine the alternative treatments as effective [1].
Resetting the gut microbiome is key to this incurable disease, in my biomedical view.
Pharmaceutical

There are many pharmaceutical options to treat IBS symptoms, such as: bulk forming (ispaghula) and laxatives for constipation, opioid receptor agonists (loperamide) for diarrhea, anti-spasmodics to treat abdominal pain.
However, pills are expensive and come with unwanted side effects [2]. Ergo, through the lenses of many experienced health professionals (eg. Dr Michael Mosley, David Perlmutter), resetting the gut microbiome via natural remedies and changing lifestyle will treat unwanted IBS symptoms.
What if Changing lifestyle does not improve my bowel irritation, abdomen and stomach pain?
Understand the most prominent symptom and bowel habit [1], then focus to treat that symptom only.
Bacterial infection: There may be a bacterial infection in the gut, so visiting the GP to receive antibiotics will ensure that staphylococcus A., Campylobacter, E.coli imbalance and many more pesky unwanted microbes are not the main source of the symptoms experienced.
Main treatment?

Stress Free: A calm body and mind, a calm gut health as it is your brain that controls digestion! Busting stress from your life is crucial.
In fact, reducing stress should be everyone’s primary priority.

Meditate, read, pray to God, yoga. Anything that can destress your body is crucial to reducing IBS associated pain. I pray 5 times a day, read and reflect on the Quran teachings.
To Treat Diarrhea and Constipation: Laxatives, prokinetics and antidiarrheals. Green tea , ginger and senna are natural remedies to treat the symptoms of constipation. Chamomile tea is best to treat diarrhea.
Regular exercise:

A 5 minute walk is more than sufficient. If you an active person, go for a jog at your park instead. If Dumbbells is more to your taste, then HIIT 15 is the way to go!
Wear looser clothing: reduces body stress
Avoiding certain foods: coffee, fruit juices and reduce the spices in your food.
£11.70 Paperback format of: The Low-FODMAP Recipe Book: Relieve Symptoms of IBS, Crohn’s Disease & Other Gut Disorders in 4–6 Weeks
Avoid gluten foods: Bread is the best tasting food to stay away from and generally follow the gluten-free low-FODMAP diet, which significantly reduces bloating, pain and irritation to your bowels [1]. No croissants, baguettes, sourdough, pastry…
Eat certain foods: gut microbiome and micrflux containing probiotics


Management By Healthcare Providers
It has been predicted via data analysis from a population based study [9]:
“Health care seeking was independently associated with severity and duration of the pain rather than psychological factors.”
source: click here
Patients that seek aid of their local GP’s resulting in hospital referrals, predominantly do not want to focus on psychological factors. Such as stress and such mental disorders. Treatment is to reduce symptoms and their severity.
Since 2016, this system of IBS management 6 months prior diagnosis has been optimised to utilise a team–effective algorithm for clinical practice [12]. Focussing not only on symptomology, but also the psychological factors associated with IBS [12].
Image below elegantly displays this new European System [13]:
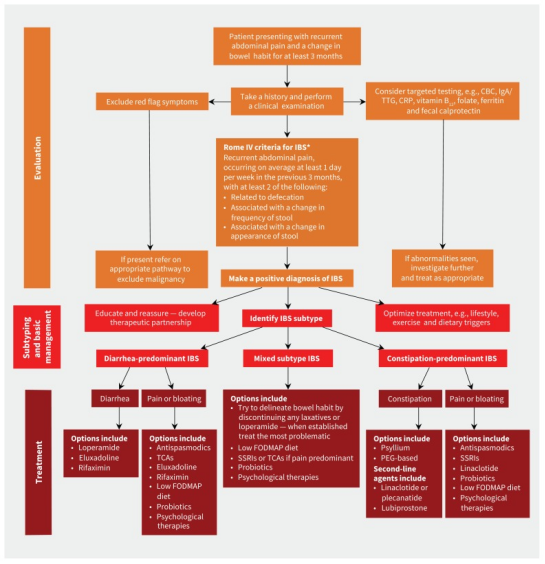
Fig.4: algorithm to display IBS management 6 months prior diagnosis within European healthcare systems.
Case studies on current situation and IBS

An important research study [3] was conducted to identify if stress was directly related to worsening symptoms of IBS. The late 2020 study did approve this hypothesis statistically for the specific geographical location. Read on.
Data was collected electronically as a questionnaire from the Saudi Arabian participants of 1255 IBS patients [3] and gathered via descriptive cross-sectional approach.
What is interesting, is that the stress caused by the pandemic specifically elevated chronic morbidities and associated symptoms of the IBS patients’ that stated worsening IBS. This accounts to 63.4% of 1255. That is nearly 2/3rds of the total patients that are stressed, COVID-19 pandemic as the culprit.

Additionally, 56.6% of those stressed explicitly stated that they experienced severe elevation of the symptoms. In other words; diarrhea, constipation, pain levels increased more than they can normally cope. Furthermore, with P = .039 and .001 respectively, more than 3/4 (75.5%) of all 1255 patients statistically approve impaired completion of their daily tasks.
Ergo, reducing stress most certainly will reduce chronic abdomen pain and all associated IBS symptoms [3].
Though this is evident, external factors such as geographical climate, diet and lifestyle specific to Saudi Arabia, must be taken into consideration. So I researched the scientific database even further!
Thus, an anonymised study collected data from 2704 individuals from 33 countries [4]. Published in the journal of gastroenterology and hepatology, this study looked not only on the IBS symptoms, but also the impact that the pandemic showcased to all individuals (IBS and non-IBS participants).
The researchers concluded that “self-reported IBS respondents had worse well-being and compliance to social distancing measures than non-IBS respondents.”
Understanding and maintaining personal hygiene, psychological impact of COVID-19 and attitude towards social distancing were evaluated statistically for all individuals.
We should all praise the researchers, as not only did they focus on IBS symptoms and association with the pandemic, but also shifted the focal lense to well-being and compliance differences between the 33 countries involved. This will give a better understanding of IBS patients overall.
305 (11.3%) of 2704 participants [4] were self-reported IBS and were analysed as being significantly worse in terms of emotional, social, and psychological well-being compared with non-IBS respondents. 28.2% IBS vs 35.3% non-IBS, with P = 0.029. 11.8% of the 305 self-reported IBS individuals experienced worsening IBS symptoms. 61.6% of 305 reported no change in symptoms. It is this group that were willing to practise social distancing indefinitely. 74.9% vs 51.4%, P = 0.016.
Thus, through multivariate analysis, this data indicates that if social distancing is followed in 3 weeks> chunks, there is an association of greater odds of improving IBS symptoms .
As Quek et al [4] stated: the follow up and future research should also focus on other factors such as occupational stress (not only pandemic stress) and dietary changes that were adapted during the COVID-19 pandemic.
Yes, but what about the vaccine? So I summarised the UK vaccine strategy below!
Now, vaccines are available in the UK. Not everyone is vaccinated mainly due to stock availability [5]. With this in mind, equitable access to COVID-19 vaccination programmes should be endorsed for patients with IBS symptoms and IBD patients.
In other words, there should be a greater emphasis on vaccinating IBD patients within the NHS preventative scheme.
This article [5] implies that NHS policy makers need to design and develop future COVID-19 vaccination programmes which includes high risk IBD patients.
Ergo, design with the knowledge of gastrointestinal health in mind.
Dietary Changes?
It is known that upper and lower respiratory diseases , such as [6] severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) virus for the latter, can affect the digestive system and present with gastrointestinal (GI) symptoms. Patients with COVID–19, SARS‐CoV‐2 virus can disrupt the mucosa of the normal intestine.
This can potentially and has resulted in many patients with GI symptoms and a compromise in nutrient absorption [6]. Specifically designed Oral diet is the recommended treatment for these patients. However, many patients lose their appetite. Therefore, this diet alone is not enough. Enteral nutrition is the preferred route to promote gut integrity and immune function [6].
This explicit evidence is sufficient enough for those in the upper part of the NHS hierarchy to acknowledge patients with gastrointestinal symptoms. Symptoms in relation to associated syndromes and diseases. IBS is one of them!
Yes, many countermeasures are used to relieve side effects of ICU COVID-19 patients that display a significant barrier in GI intolerance. However, the threshold for the allowed use of parenteral nutritional should be lower [6] than the current level.
To recap on the virus understanding:
SARS‐CoV‐2, is an enveloped RNA betacoronavirus that attaches to the angiotensin‐converting enzyme 2 (ACE2) receptor. Thus, the virus is allowed to enter the target cell and as a result, facilitate replication and cause death amongst the lower respiratory lining.
However, ACE2 receptors are abundantly available throughout the digestive system. The significant number of these receptors are located within the enterocytes, lining of the ileum and colon. That is the same locus in which IBS symptoms, pain and large intestine discomfort of the tissues are experienced. SARS-CoV-2 uses ACE2 and the serine protease TMPRSS2 for S protein priming. ACE2 and the protease are expressed in the lungs and small intestinal epithelia.
Yet, no study on IBS [7]!
Yet, D’Amico and his researchers [8] have focussed on diarrhea and COVID-19. They found that management of viral infections, healthcare systems are utilising the knowledge of biomedical science, in relation to patients’ gut microbiome. [8] Probiotics have been proposed for patients with COVID‐19, according to these researchers.
Though the focus is to treat diarrhea, it is a great sign for the medical sector and opens doors to new therapeutic opportunities.
Such targets in which medications (antibiotics and antivirals) and certain treatments (probiotics, dietry, yakult, fermented food items) are prescribed to improve the gut microbiota of patients with diarrhea and COVID-19. This will aid our future understanding of IBS in relation to its treatment. Regardless of any virus pandemic!
IBS Shopping List:

£11.99 Low Formal Diet For Beginners 7-day plan
£6.27 The Clever Guts Diet by Dr Michael Mosley
£2.69 Clipper Fair Trade Green Tea
£20 for 6 pack, 480 Clipper fairtrade Green Tea
Be sure to check out below for my other posts and all the links to the products I use recommended within this post.
Don’t forget to comment below and share this blog (below icons if on mobile or on the side if on the laptop) to friends and family, it will be greatly appreciated by me and your loved ones. Stay Safe!
ADDITIONAL SOURCES and Recommened Products:
[1] Masuy, I., Pannemans, J., & Tack, J. (2020). Irritable bowel syndrome: diagnosis and management. Minerva gastroenterologica e dietologica, 66(2), 136–150. https://doi.org/10.23736/S1121-421X.19.02640-0
[2] CMAJ. 2020 Mar 16; 192(11): E275–E282. doi: 10.1503/cmaj.190716 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7083544/
[3] Medicine (Baltimore). 2020 Dec 18; 99(51): e23711. Published online 2020 Dec 18. doi: 10.1097/MD.0000000000023711 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7748344/
[4] Quek, Sabrina Xin Zi et al. “Impact of the coronavirus disease 2019 pandemic on irritable bowel syndrome.” Journal of gastroenterology and hepatology, 10.1111/jgh.15466. 21 Feb. 2021, doi:10.1111/jgh.15466 https://pubmed.ncbi.nlm.nih.gov/33615534/
[5] Lancet Gastroenterol Hepatol. 2020 Nov; 5(11): 965–966. Published online 2020 Sep 21. doi: 10.1016/S2468-1253(20)30295-8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7505629/
[6] Nutr Clin Pract. 2020 Jul 15 : 10.1002/ncp.10554. doi: 10.1002/ncp.10554 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7405319/
[7] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7405319/#ncp10554-bib-0004
[8] D’Amico F, Baumgart DC, Danese S, Peyrin‐Biroulet L. Diarrhea during COVID‐19 infection: pathogenesis, epidemiology, prevention and management. Clin Gastroenterol Hepatol. 2020;18(8):1663‐1672. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7141637/?report=reader
[9] Talley NJ, Boyce PM, Jones M. Predictors of health care seeking for irritable bowel syndrome: a population based study. Gut 1997;41:394–8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1891476/?report=reader
[10] De Palma G, Collins SM, Bercik P. The microbiota-gut-brain axis in functional gastrointestinal disorders. Gut Microbes 2014;5:419–29. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4153782/?report=reader
[11] Marshall JK, Thabane M, Garg AX, et al. Walkerton Health Study Investigators. Incidence and epidemiology of irritable bowel syndrome after a large waterborne outbreak of bacterial dysentery. Gastroenterology 2006;131:445–50, quiz 660 https://www.ncbi.nlm.nih.gov/pubmed/16890598
[12] IBS Management figure with symptoms 6 months prior diagnosis: Moayyedi P, Mearin F, Azpiroz F, et al. Irritable bowel syndrome diagnosis and management: a simplified algorithm for clinical practice. United European Gastroenterol J 2017;5:773–88. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5625880/?report=reader
[13] Figure for Management: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7083544/figure/f3-192e275/?report=objectonly


Perfect just what I was searching for! .
Needed to put you this bit of word so as to thank you so much over again about the wonderful secrets you’ve discussed on this page. This is simply wonderfully open-handed with you to grant unhampered precisely what many individuals would’ve distributed as an e book to end up making some money for their own end, particularly now that you could possibly have done it in the event you considered necessary. These guidelines in addition worked to be a fantastic way to comprehend other individuals have the identical dream the same as my own to know great deal more with reference to this problem. I believe there are millions of more pleasurable moments ahead for individuals who find out your site.
Good blog! I really love how it is easy on my eyes and the data are well written. I’m wondering how I might be notified whenever a new post has been made. I have subscribed to your RSS feed which must do the trick! Have a nice day!
Terrific work! This is the type of information that should be shared around the web. Shame on Google for not positioning this post higher! Come on over and visit my website . Thanks =)
Thank you. What is your website?
great submit, very informative. I ponder why the other experts of this sector don’t notice this. You must proceed your writing. I’m confident, you have a huge readers’ base already!
Thank you for your feedback. Few have noticed, but many healthcare and like-minded professionals have not encountered my articles. I will focus on marketing my posts in the near future.
I’m also commenting to let you understand of the fine experience my cousin’s daughter encountered going through yuor web blog. She mastered lots of issues, including what it’s like to possess an awesome teaching heart to get the rest smoothly know precisely a number of impossible topics. You really did more than her expectations. Many thanks for giving such warm and friendly, healthy, educational as well as unique tips on this topic to Mary.
I am only writing to let you be aware of of the wonderful experience my friend’s girl went through reading through your site. She discovered some pieces, which included what it is like to possess a marvelous teaching style to let many others smoothly learn about a variety of complicated subject areas. You truly did more than readers’ desires. I appreciate you for rendering such great, dependable, edifying and as well as unique tips on the topic to Evelyn.
It抯 laborious to search out knowledgeable individuals on this matter, however you sound like you know what you抮e talking about! Thanks
Thanks.Saf